- Details
As an intermediary step, EDI-Laravel Framework converts an incoming EDI file to JSON. From there, most programmers can figure out how to get that data into your database, feed it to your ERP or other management systems.
If your company is new to EDI, you might not realize how much work you will save by using the EDI-Laravel framework, so let's show you an example.
Here's a very small EDI file. It's a 210 so it's an invoice for freight charges. It only contains one invoice.
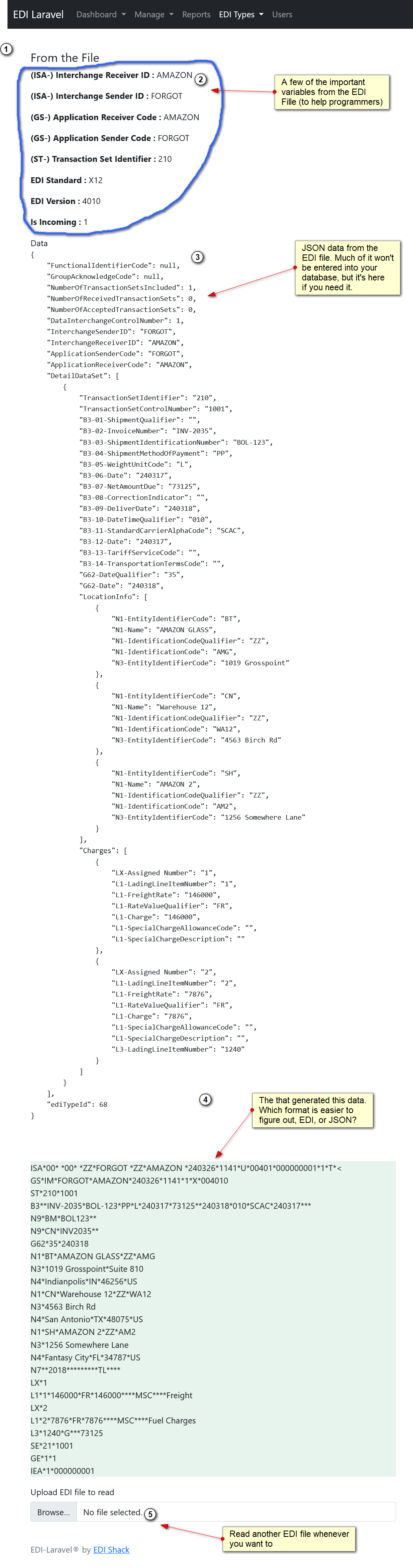
That's a screen shot from the EDI-Laravel Framework after manually reading a small EDI file. It shows a few variables pulled from the file, then the data pulled from the file, and finally the file itself.
- Details
NOTE - All new HIPAA EDI Transactions should be X12 5010 Version
A lot of EDI providers make a huge deal of the security provisions of the HIPAA act, but please, don't worry about it. All HIPAA really says is that EDI transactions must be secure, and EDI Transactions have almost always been secure anyway. It's probably best to use FTPS, SFTP, HTTPS, or AS2 instead of just plain FTP though. FTP has never been that secure, but the other transmission protocols are secure, and easy to use.
835: Health Care Claim Payment/Advice.
The 835 Health Care Payment / Advice, also known as the Electronic Remittance Advice (ERA), provides information for the payee regarding claims in their final status, including information about the payee, the payer, the payment amount, and any payment identifying information. An 835 is sent from insurers to the healthcare providers.
837: Health Care Claim.
To put it simply… the 835 is the receipt and the 837 is a bill. An 835 claim file is the format that insurance organizations send back to healthcare providers.
• 834: Benefit Enrollment and Maintenance.
• 820: Premium billing (Receipt).
• 278: Request for review and response.
• 270/271: Health Care Eligibility Benefit Inquiry and Response.
• 276/277: Health Care Claim Status Request and Response.
• 997: Functional Acknowledgement; TA1-Interchange Acknowledgement.
• 999: Acceptance/Rejection Advice.
- Details
The Health Insurance Portability and Accountability Act was enacted by the U.S congress in 1996. A key component of HIPAA is the establishment of national standards for electronic health care transactions and national identifiers for providers, health insurance plans and employers.
The standards are meant to improve the efficiency and effectiveness of the North American health care system by encouraging the widespread use of EDI in the U.S health care system.
NOTE - The HIPAA EDI transaction sets are based on X12, version 5010
The key message types are described below:
837 - EDI Health Care Claim
The 837 is usually the first transaction set you will need to implement. It's used to submit health care claim billing information, encounter information, or both, except for retail pharmacy claims (see EDI Retail Pharmacy Claim Transaction). It can be sent from providers of health care services to payers, either directly or via intermediary billers and claims clearinghouses. It can also be used to transmit health care claims and billing payment information between payers with different payment responsibilities where coordination of benefits is required or between payers and regulatory agencies to monitor the rendering, billing, and/or payment of health care services within a specific health care/insurance industry segment.
The 837 is a relatively complicated transaction set, but it comes in 2 different flavors which helps simplify it slightly. There are 837 Institutional (“I”) and 837 Professional (“P”) transactions. They are both based on the standard 837, but do not include all possible variations of the 837.
835 - Health Care Claim Payment/Remit Advice
Can be used to make a payment, send an Explanation of Benefits (EOB) remittance advice, or make a payment and send an EOB remittance advice only from a health insurer to a health care provider either directly or via a financial institution.
270/271 - Inquiry/Response for Eligibility
Allows determination of subscriber or dependent eligibility as well as the benefit information for the subscriber or dependent. The 270 is sent to a health plan to determine the eligibility, or benefit availability. The 271 is the eligibility/benefit response. Because this information can be critical, many health plans make these interactive or real time.
276/277 - Inquiry/Response for Claim Status
Used by providers to request status on a submitted claim (276) and to receive a status response (277). The 276 is utilized by institutional, professional and dental providers, and supplemental health care claims processors as defined by the regulations. The 277 response transactions are utilized by payers and other entities that process claims.
278 - Referral Certification, Authorization, Extensions and Appeals
Referral Certification: Used by providers to request certification for a patient to receive health care services. Also provides capacity to appeal a UM decision. Authorization: Provider receives permission from review entity/UM to refer the patient to a specialist, admit the patient to a facility, or administer medical services or treatment to the patient. This transaction also covers pre-certification prior to elective hospitalization or treatment, as required, for determination of medical necessity. This transaction allows the provider to request an extension to a previously approved authorization, pre-certification, or referral. The 278 is implemented as an interactive transaction.
Below are all the possible X12 transactions for Healthcare including all HIPAA
The key X12 EDI transaction sets for Healthcare including HIPAA are:
-
- EDI 270 Eligibility, Coverage or Benefit Inquiry
- EDI 271 Eligibility, Coverage or Benefit Information
- EDI 275 Patient Information
- EDI 276 Healthcare Claim Status Request
- EDI 277 Healthcare Claim Status Notification
- EDI 278 Healthcare Services Review – Request for Review
- EDI 278 Healthcare Services Review – Response to Request for Review
- EDI 820 Payment Order/Remittance Advice
- EDI 824 Format Example
- EDI 834 Benefit Enrollment and Maintenance
- EDI 835 Healthcare Claim Payment/Advice
- EDI 837-P Healthcare Claim: Professional
- EDI 837-D Healthcare Claim: Dental
- EDI 837-I Healthcare Claim: Institutional
- EDI 997 Functional Acknowledgment for Healthcare Insurance
- EDI 999 Implementation Acknowledgment for Healthcare Insurance
- EDI TA1 Interchange Acknowledgment
(Note: As of 2012, healthcare providers must be compliant with version 5010 of the HIPAA EDI standards.)
Any entities covered by the HIPAA EDI Rule should be aware that penalties for non-compliance are high. There are 4 tiers of non-compliance:
- Tier 1, which refers to unknowing violations
- Tier 2, which refers to a reasonable cause for violations
- Tier 3, which refers to willful violations that have been corrected
- Tier 4, which refers to willful violations that have not been corrected
The penalties for the last tier are the highest, with a minimum penalty of $50,000 per violation.
- Details
There seems to be nothing in the IT world that is more important to a company, and yet causes so much confusion for Business Managers, IT Managers, and the entire IT department than EDI. If a company needs EDI, then EDI quickly becomes the most important process in the chain.
My own personal search for EDI Mastery started in 2001, I think around August of 2001. The company I was working for was taking on another major customer that would account for about 50% of the total business of my company. We were based in Detroit, and the new customer was one of the Big 3 car companies, and the process we were managing for them helped keep their factories running, and could easily shut down a factory if it went wrong. Needless to say it was important, and a lot of jobs depended on getting it right.
The implementation managers had been working with the car company for several months to get everything working, and then creating training materials and getting staff up to speed on how it worked. In a meeting a few weeks before the launch, the car company rep mentioned that we had to send on-time updates to them via EDI to get paid. Suddenly EDI was very important to the entire management team, and my manager, the IT department head, got pulled into a meeting and was told "We don't know what EDI is, but here are some specs on it, and we need it working 6 weeks from now". It was then passed on to me. I knew it was important to get right, but I didn't know anything about EDI except that it was some form of text file, and companies sent data to and from other companies with it. I decided the only way I would be able to get this done was to spend 3 weeks learning about EDI and the final 3 weeks programming.
- Details
EDIFACT: The universal message standard
What is EDIFACT?
EDIFACT is the abbreviation for "Electronic Data Interchange for Administration, Commerce and Transport". This is a global set of rules defined by the UN for the inter-company electronic data exchange between two or more business partners via EDI.
It should be noted that EDIFACT is a newer standard for EDI than ANSII X12. X12 is mainly used in America, while EDIFACT is a world-wide standard.
The goal of EDIFACT is the optimization and standardization of the data flow between business partners. By defining uniform segments and elements that describe the information in the electronic file and which are used for a wide variety of document types (such as invoices, purchase orders, delivery notes, etc.) merely by means of a differentiated arrangement, a worldwide standard was created.
However, the EDIFACT standard is very comprehensive and created for almost every business transaction and every industry, subgroups (the so-called subsets) soon emerged. The subset EANCOM was created for the retail sector, which contains the mandatory fields of the EDIFACT standard and the industry-specific optional fields. By creating so-called subsets, the messages are better handled and easier to understand.
- Details
You run a small business, let's say an online store on Shopify. Several of your suppliers have EDI capabilities, and it's obvious to you that some of your processes can be automated if you just knew what EDI is.
EDI is short for "Electronic Document Interface", and it's an accurate description. EDI is a system for exchanging documents between companies in a clear, precise format that eliminates errors and misunderstandings. EDI can be easily automated. However, EDI must be done correctly, or it can be a nightmare.
Imagine you have a small company that sells custom laptops to consumers. Amazon does your shipping for you, so everyday you send dozens of laptops to the Amazon warehouse, and you take orders on your Amazon store and website. Currently, everytime you sell a laptop, you have to enter the information into a form to send it to Amazon. Not only is this system prone to data entry errors, it's time consuming. You decide to automate this, so you hire someone to create an EDI file and send it to Amazon. What you have to realize about EDI is it's automated. Nobody is looking to make sure the data is correct before it's sent to your trading partner. In this case, what if every order gets tripled? What if some orders are never sent? If the orders get tripled, how long can you stay in business if Amazon ships 3 of every laptop you've sold? how many customers will you lose if the order gets lost? When you setup EDI, your system needs to have a mechanism to be 100% sure every order is sent once, and only once. Thankfully, automated EDI makes a LOT fewer mistakes than manual data entry, and eventually automated EDI will make zero mistakes if you maintain it properly. Amazon will of course send back a 997 for every order in an EDI file. The 997 will tell you whether the information you sent was accepted by Amazon. However, your system has to be capable of matching the incoming information from Amazon to the data in your system.
Although an EDI document is simply a text file in EDI format, EDI is MUCH, MUCH MORE than that. EDI is a document management system that specifies how to manage your files, keep track of which documents were received by your trading partner, whether the data was successfully extracted by the EDI system, and whether the data was successfully used. No other document does all that. If you combined a very good document management system and then integrated a file format into it, and then consulted with every major industry on what information they need to share, that's what EDI is.
The EDI file format has wrappers that if properly used, keeps track of not only the file in question, but the files that came before it.
Here's a small checklist of what your EDI system has to do (using the example above). Note that creating the actual EDI file is only a small part of the total.
- Pull the data for all new orders once an hour, or once a day (whatever your timeline is)
- make sure to ONLY pull the information for paid orders
- check for missing information. EDI should NEVER send incomplete information
- notify staff if there are orders completed, but still missing information
- using the data pulled, format it into EDI formats
- Compose the EDI file
- Store the EDI file in long term storage
- put a copy of the EDI file in a directory you will send from
- Start the sending system so the file gets sent to your trading partner
- Verify the file was sent properly, AND received by the trading partner
- Check to see if there are any reply files that need to be read
- for every reply file, match the data to your data and update the entries
- Close down properly without any memory leaks
Note that composing the EDI file is about halfway in the total process and there are a lot of things to be done BEFORE and AFTER the file is actually composed
